
New York State shattered a 21-year public health record during the week ending December 20, 2025, reporting 71,123 laboratory-confirmed influenza cases—the highest weekly total since the disease became reportable in 2004. State Health Commissioner Dr. James McDonald confirmed the unprecedented surge represents a 38% increase from the prior week, instantly elevating concerns about healthcare system capacity as the traditional peak flu months of January and February still loom ahead. The outbreak has pushed the season’s cumulative total to 189,312 confirmed cases statewide, with hospitalizations climbing at an even more alarming rate than infections themselves.
Healthcare Systems Under Mounting Pressure

Alongside the record case count, New York documented a 63% surge in flu-related hospitalizations within the same week, jumping from 2,251 to 3,666 admissions statewide. The hospitalization spike confirms the outbreak extends beyond mild illness, placing acute strain on hospital emergency departments and inpatient units already managing routine care demands.
By the following week ending December 27, hospitalizations reached an even higher record of 4,546—nearly 1,000 more patients than the previous seven-day period. McDonald noted that officials are “closely reviewing hospital bed capacity data to better understand hospitalization trends and to guide any necessary response related to impacts from respiratory viral infections.” The rapid escalation means even facilities operating with adequate staffing face mounting challenges as patient volumes continue climbing.
A New Viral Variant Driving Transmission
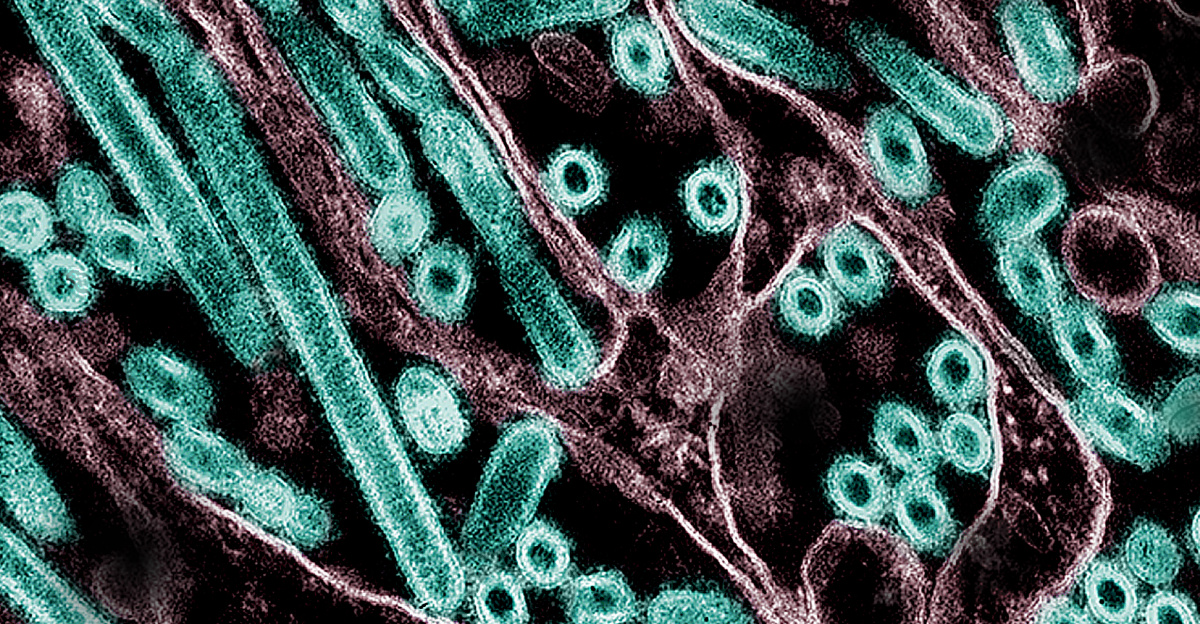
Epidemiologists have identified the dominant strain fueling this season’s surge as H3N2 subclade K, a mutated variant of influenza A that features significant genetic changes in its surface proteins. These mutations allow the virus to partially evade immune defenses generated by previous infections or vaccinations, increasing transmission efficiency across populations with only partial immunity. Subclade K emerged during the summer of 2025 and drove severe early-season outbreaks in countries including the United Kingdom, Japan, and Australia before spreading rapidly through the United States.
Nearly 90% of H3N2 samples analyzed by the Centers for Disease Control and Prevention since September belong to this subclade. While current evidence suggests subclade K does not cause more severe disease than other flu strains, its enhanced ability to spread through communities—even among vaccinated individuals—explains the unprecedented velocity of New York’s outbreak. The vaccine still provides meaningful protection against severe illness and hospitalization, though effectiveness against infection appears reduced compared to better-matched seasons.
Policy Response and Vulnerable Populations

On December 2, 2025, New York officially declared influenza “prevalent statewide,” triggering enhanced public health protocols under state sanitary code. The declaration mandates that all healthcare personnel who have not received the current season’s flu vaccine must wear surgical or procedure masks in patient-care areas. This requirement aims to limit transmission within hospitals, clinics, and residential facilities where vulnerable populations face heightened risk of severe outcomes.
Children, pregnant individuals, adults over 65, and those with chronic medical conditions or weakened immune systems remain most susceptible to complications requiring hospitalization. Officials emphasize that antiviral medications such as oseltamivir remain effective against subclade K when initiated within 48 hours of symptom onset, making early recognition and prompt medical consultation critical as community transmission intensifies. McDonald stressed that “flu is treatable for high-risk people with antiviral medicine, if taken within 48 hours of symptoms.”
Looking Ahead Through Peak Season

The timing of New York’s record-breaking week raises particular concern among public health officials because historical patterns show flu activity often peaks in late December through February, not mid-December. Current infection rates may not represent the season’s worst phase, meaning hospitalizations could climb further in coming weeks. With approximately one in every 275 New Yorkers testing positive during the record week alone, widespread community exposure has become increasingly difficult to avoid across workplaces, schools, and households.
Officials continue urging practical protective measures: staying home when symptomatic, seeking testing and treatment promptly, and limiting exposure around vulnerable individuals. While vaccination rates have declined compared to previous seasons—only 42% of adults nationwide had received flu shots as of mid-December—health authorities stress it remains beneficial to get vaccinated even this late in the season. The outbreak serves as a stark reminder that influenza can overwhelm healthcare systems when viral evolution, reduced immunity, and seasonal timing converge, underscoring the need for sustained vigilance as winter progresses.
Sources
“New York Department of Health announces most flu cases ever recorded in 1 week.” ABC7NY / WABC, 28 Dec 2025.
“Record-breaking flu numbers reported in New York state, sparking warnings from officials.” Fox News, 27 Dec 2025.
“New York reports record-breaking number of flu hospitalizations in a single week.” ABC News, 1 Jan 2026.
“New York City breaks a flu record as 2025 cases surge, state health officials say.” CBS News New York, 27 Dec 2025.